Type 2 diabetes—the most common form of diabetes—is caused by a combination of factors, including insulin resistance, a condition in which the body’s muscle, fat, and liver cells do not use insulin effectively. Type 2 diabetes develops when the body can no longer produce enough insulin to compensate for the impaired ability to use insulin. Symptoms of type 2 diabetes may develop gradually and can be subtle; some people with type 2 diabetes remain undiagnosed for years.
Type 2 diabetes develops most often in middle-aged and older people who are also overweight or obese. The disease, once rare in youth, is becoming more common in overweight and obese children and adolescents. Scientists think genetic susceptibility and environmental factors are the most likely triggers of type 2 diabetes.
Genetic Susceptibility
Genes play a significant part in susceptibility to type 2 diabetes. Having certain genes or combinations of genes may increase or decrease a person’s risk for developing the disease. The role of genes is suggested by the high rate of type 2 diabetes in families and identical twins and wide variations in diabetes prevalence by ethnicity. Type 2 diabetes occurs more frequently in African Americans, Alaska Natives, American Indians, Hispanics/Latinos, and some Asian Americans, Native Hawaiians, and Pacific Islander Americans than it does in non-Hispanic whites.
Recent studies have combined genetic data from large numbers of people, accelerating the pace of gene discovery. Though scientists have now identified many gene variants that increase susceptibility to type 2 diabetes, the majority have yet to be discovered. The known genes appear to affect insulin production rather than insulin resistance. Researchers are working to identify additional gene variants and to learn how they interact with one another and with environmental factors to cause diabetes.
Studies have shown that variants of the TCF7L2 gene increase susceptibility to type 2 diabetes. For people who inherit two copies of the variants, the risk of developing type 2 diabetes is about 80 percent higher than for those who do not carry the gene variant.1However, even in those with the variant, diet and physical activity leading to weight loss help delay diabetes, according to the Diabetes Prevention Program (DPP), a major clinical trial involving people at high risk.
Genes can also increase the risk of diabetes by increasing a person’s tendency to become overweight or obese. One theory, known as the “thrifty gene” hypothesis, suggests certain genes increase the efficiency of metabolism to extract energy from food and store the energy for later use. This survival trait was advantageous for populations whose food supplies were scarce or unpredictable and could help keep people alive during famine. In modern times, however, when high-calorie foods are plentiful, such a trait can promote obesity and type 2 diabetes.
Obesity and Physical Inactivity
Physical inactivity and obesity are strongly associated with the development of type 2 diabetes. People who are genetically susceptible to type 2 diabetes are more vulnerable when these risk factors are present.
An imbalance between caloric intake and physical activity can lead to obesity, which causes insulin resistance and is common in people with type 2 diabetes. Central obesity, in which a person has excess abdominal fat, is a major risk factor not only for insulin resistance and type 2 diabetes but also for heart and blood vessel disease, also called cardiovascular disease (CVD). This excess“belly fat” produces hormones and other substances that can cause harmful, chronic effects in the body such as damage to blood vessels.
The DPP and other studies show that millions of people can lower their risk for type 2 diabetes by making lifestyle changes and losing weight. The DPP proved that people with prediabetes—at high risk of developing type 2 diabetes—could sharply lower their risk by losing weight through regular physical activity and a diet low in fat and calories. In 2009, a follow-up study of DPP participants—the Diabetes Prevention Program Outcomes Study (DPPOS)—showed that the benefits of weight loss lasted for at least 10 years after the original study began.
More information about the DPP, funded under National Institutes of Health (NIH) clinical trial number NCT00004992; the DPPOS, funded under NIH clinical trial number NCT00038727; and other studies related to type 2 diabetes is available in the following NDIC fact sheets at www.diabetes.niddk.nih.gov:
- Diabetes Overview
- Diabetes Prevention Program
Insulin Resistance
Insulin resistance is a common condition in people who are overweight or obese, have excess abdominal fat, and are not physically active. Muscle, fat, and liver cells stop responding properly to insulin, forcing the pancreas to compensate by producing extra insulin. As long as beta cells are able to produce enough insulin, blood glucose levels stay in the normal range. But when insulin production falters because of beta cell dysfunction, glucose levels rise, leading to prediabetes or diabetes.
Abnormal Glucose Production by the Liver
In some people with diabetes, an abnormal increase in glucose production by the liver also contributes to high blood glucose levels. Normally, the pancreas releases the hormone glucagon when blood glucose and insulin levels are low. Glucagon stimulates the liver to produce glucose and release it into the bloodstream. But when blood glucose and insulin levels are high after a meal, glucagon levels drop, and the liver stores excess glucose for later, when it is needed. For reasons not completely understood, in many people with diabetes, glucagon levels stay higher than needed. High glucagon levels cause the liver to produce unneeded glucose, which contributes to high blood glucose levels. Metformin, the most commonly used drug to treat type 2 diabetes, reduces glucose production by the liver.
The Roles of Insulin and Glucagon in Normal Blood Glucose Regulation
A healthy person’s body keeps blood glucose levels in a normal range through several complex mechanisms. Insulin and glucagon, two hormones made in the pancreas, help regulate blood glucose levels:
- Insulin, made by beta cells, lowers elevated blood glucose levels.
- Glucagon, made by alpha cells, raises low blood glucose levels.
When blood glucose levels rise after a meal, the pancreas releases insulin into the blood.
- Insulin helps muscle, fat, and liver cells absorb glucose from the bloodstream, lowering blood glucose levels.
- Insulin stimulates the liver and muscle tissue to store excess glucose. The stored form of glucose is called glycogen.
- Insulin also lowers blood glucose levels by reducing glucose production in the liver.
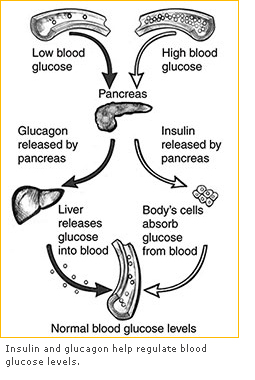 When blood glucose levels drop overnight or due to a skipped meal or heavy exercise, the pancreas releases glucagon into the blood.
When blood glucose levels drop overnight or due to a skipped meal or heavy exercise, the pancreas releases glucagon into the blood.
- Glucagon signals the liver and muscle tissue to break down glycogen into glucose, which enters the bloodstream and raises blood glucose levels.
- If the body needs more glucose, glucagon stimulates the liver to make glucose from amino acids.
Metabolic Syndrome
Metabolic syndrome, also called insulin resistance syndrome, refers to a group of conditions common in people with insulin resistance, including
- higher than normal blood glucose levels
- increased waist size due to excess abdominal fat
- high blood pressure
- abnormal levels of cholesterol and triglycerides in the blood
People with metabolic syndrome have an increased risk of developing type 2 diabetes and CVD. Many studies have found that lifestyle changes, such as being physically active and losing excess weight, are the best ways to reverse metabolic syndrome, improve the body’s response to insulin, and reduce risk for type 2 diabetes and CVD.
Cell Signaling and Regulation
Cells communicate through a complex network of molecular signaling pathways. For example, on cell surfaces, insulin receptor molecules capture, or bind, insulin molecules circulating in the bloodstream. This interaction between insulin and its receptor prompts the biochemical signals that enable the cells to absorb glucose from the blood and use it for energy.
Problems in cell signaling systems can set off a chain reaction that leads to diabetes or other diseases. Many studies have focused on how insulin signals cells to communicate and regulate action. Researchers have identified proteins and pathways that transmit the insulin signal and have mapped interactions between insulin and body tissues, including the way insulin helps the liver control blood glucose levels. Researchers have also found that key signals also come from fat cells, which produce substances that cause inflammation and insulin resistance.
This work holds the key to combating insulin resistance and diabetes. As scientists learn more about cell signaling systems involved in glucose regulation, they will have more opportunities to develop effective treatments.
Beta Cell Dysfunction
Scientists think beta cell dysfunction is a key contributor to type 2 diabetes. Beta cell impairment can cause inadequate or abnormal patterns of insulin release. Also, beta cells may be damaged by high blood glucose itself, a condition called glucose toxicity.
Scientists have not determined the causes of beta cell dysfunction in most cases. Single gene defects lead to specific forms of diabetes called maturity-onset diabetes of the young (MODY). The genes involved regulate insulin production in the beta cells. Although these forms of diabetes are rare, they provide clues as to how beta cell function may be affected by key regulatory factors. Other gene variants are involved in determining the number and function of beta cells. But these variants account for only a small percentage of type 2 diabetes cases. Malnutrition early in life is also being investigated as a cause of beta cell dysfunction. The metabolic environment of the developing fetus may also create a predisposition for diabetes later in life.
Risk Factors for Type 2 Diabetes
People who develop type 2 diabetes are more likely to have the following characteristics:
- age 45 or older
- overweight or obese
- physically inactive
- parent or sibling with diabetes
- family background that is African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, or Pacific Islander American
- history of giving birth to a baby weighing more than 9 pounds
- history of gestational diabetes
- high blood pressure—140/90 or above—or being treated for high blood pressure
- high-density lipoprotein (HDL), or good, cholesterol below 35 milligrams per deciliter (mg/dL), or a triglyceride level above 250 mg/dL
- polycystic ovary syndrome, also called PCOS
- prediabetes—an A1C level of 5.7 to 6.4 percent; a fasting plasma glucose test result of 100–125 mg/dL, called impaired fasting glucose; or a 2-hour oral glucose tolerance test result of 140–199, called impaired glucose tolerance
- acanthosis nigricans, a condition associated with insulin resistance, characterized by a dark, velvety rash around the neck or armpits
- history of CVD
The American Diabetes Association (ADA) recommends that testing to detect prediabetes and type 2 diabetes be considered in adults who are overweight or obese and have one or more additional risk factors for diabetes. In adults without these risk factors, testing should begin at age 45.
Grant RW, Moore AF, and Florez JC. Genetic architecture of type 2 diabetes: recent progress and clinical implications. Diabetes Care. 2009;32(6):1107–1114.
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study.Lancet. 2009;374(9702):1677–1686.