What Is Coronary Heart Disease?
Coronary heart disease (CHD) is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
When plaque builds up in the arteries, the condition is called atherosclerosis (ATH-er-o-skler-O-sis). The buildup of plaque occurs over many years.
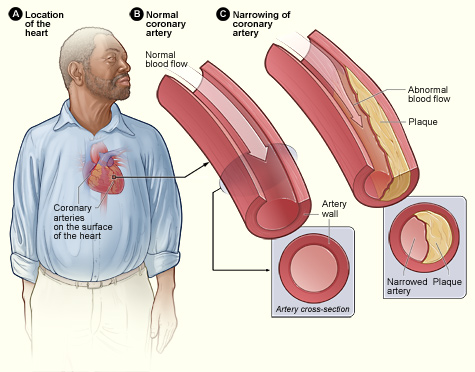
Figure A shows the location of the heart in the body. Figure B shows a normal coronary artery with normal blood flow. The inset image shows a cross-section of a normal coronary artery. Figure C shows a coronary artery narrowed by plaque. The buildup of plaque limits the flow of oxygen-rich blood through the artery. The inset image shows a cross-section of the plaque-narrowed artery.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart.
If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. Over time, ruptured plaque also hardens and narrows the coronary arteries.
Overview
If the flow of oxygen-rich blood to your heart muscle is reduced or blocked, angina (an-JI-nuh or AN-juh-nuh) or a heart attack can occur.
Angina is chest pain or discomfort. It may feel like pressure or squeezing in your chest. The pain also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion.
A heart attack occurs if the flow of oxygen-rich blood to a section of heart muscle is cut off. If blood flow isn’t restored quickly, the section of heart muscle begins to die. Without quick treatment, a heart attack can lead to serious health problems or death.
Over time, CHD can weaken the heart muscle and lead to heart failure and arrhythmias (ah-RITH-me-ahs). Heart failure is a condition in which your heart can't pump enough blood to meet your body’s needs. Arrhythmias are problems with the rate or rhythm of the heartbeat.
What Causes Coronary Heart Disease?
Research suggests that coronary heart disease (CHD) starts when certain factors damage the inner layers of the coronary arteries. These factors include:
- Smoking.
- High levels of certain fats and cholesterol in the blood.
- High blood pressure.
- High levels of sugar in the blood due to insulin resistance or diabetes.
- Blood vessel inflammation
Plaque might begin to build up where the arteries are damaged. The buildup of plaque in the coronary arteries may start in childhood.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause angina (chest pain or discomfort).
If the plaque ruptures, blood cell fragments called platelets (PLATE-lets) stick to the site of the injury. They may clump together to form blood clots.
Blood clots can further narrow the coronary arteries and worsen angina. If a clot becomes large enough, it can mostly or completely block a coronary artery and cause a heart attack.
Who Is at Risk for Coronary Heart Disease?
In the United States, coronary heart disease (CHD) is the #1 cause of death for both men and women. Each year, more than 400,000 Americans die from CHD.
Certain traits, conditions, or habits may raise your risk for CHD. The more risk factors you have, the more likely you are to develop the disease.
You can control many risk factors, which may help prevent or delay CHD.
Major Risk Factors
- Unhealthy blood cholesterol levels: This includes high LDL cholesterol (sometimes called “bad” cholesterol) and low HDL cholesterol (sometimes called “good” cholesterol).
- High blood pressure: Blood pressure is considered high if it stays at or above 140/90 mmHg over time. If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
- Smoking: Smoking can damage and tighten blood vessels, lead to unhealthy cholesterol levels, and raise blood pressure. Smoking also can limit how much oxygen reaches the body's tissues.
- Insulin resistance: This condition occurs if the body can't use its own insulin properly. Insulin is a hormone that helps move blood sugar into cells where it's used for energy. Insulin resistance may lead to diabetes.
- Diabetes: With this disease, the body's blood sugar level is too high because the body doesn't make enough insulin or doesn't use its insulin properly.
- Overweight or obesity: The terms “overweight” and “obesity” refer to body weight that’s greater than what is considered healthy for a certain height.
- Metabolic syndrome: Metabolic syndrome is the name for a group of risk factors that raises your risk for CHD and other health problems, such as diabetes and stroke.
- Lack of physical activity: Being physically inactive can worsen other risk factors for CHD, such as unhealthy blood cholesterol levels, high blood pressure, diabetes, and overweight or obesity.
- Unhealthy diet: An unhealthy diet can raise your risk for CHD. Foods that are high in saturated and trans fats, cholesterol, sodium (salt), and sugar can worsen other risk factors for CHD.
- Older age: Genetic or lifestyle factors cause plaque to build up in your arteries as you age. By the time you're middle-aged or older, enough plaque has built up to cause signs or symptoms. In men, the risk for CHD increases after age 45. In women, the risk for CHD increases after age 55.
- Family history of early heart disease. Your risk increases if your father or a brother was diagnosed with CHD before 55 years of age, or if your mother or a sister was diagnosed with CHD before 65 years of age.
Although older age and a family history of early heart disease are risk factors, it doesn't mean that you’ll develop CHD if you have one or both. Controlling other risk factors often can lessen genetic influences and help prevent CHD, even in older adults.
Emerging Risk Factors
Researchers continue to study other possible risk factors for CHD.
High levels of a protein called C-reactive protein (CRP) in the blood may raise the risk of CHD and heart attack. High levels of CRP are a sign of inflammation in the body.
Inflammation is the body's response to injury or infection. Damage to the arteries' inner walls may trigger inflammation and help plaque grow.
Research is under way to find out whether reducing inflammation and lowering CRP levels also can reduce the risk of CHD and heart attack.
High levels of triglycerides (tri-GLIH-seh-rides) in the blood also may raise the risk of CHD, especially in women. Triglycerides are a type of fat.
Other Risks Related to Coronary Heart Disease
Other conditions and factors also may contribute to CHD, including:
- Sleep apnea: Sleep apnea is a common disorder in which you have one or more pauses in breathing or shallow breaths while you sleep. Untreated sleep apnea can increase your risk for high blood pressure, diabetes, and even a heart attack or stroke.
- Stress: Research shows that the most commonly reported "trigger" for a heart attack is an emotionally upsetting event, especially one involving anger.
- Alcohol: Heavy drinking can damage the heart muscle and worsen other CHD risk factors. Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day.
- Preeclampsia (pre-e-KLAMP-se-ah): This condition can occur during pregnancy. The two main signs of preeclampsia are a rise in blood pressure and excess protein in the urine. Preeclampsia is linked to an increased lifetime risk of heart disease, including CHD, heart attack, heart failure, and high blood pressure.
What Are the Signs and Symptoms of Coronary Heart Disease?
A common symptom of coronary heart disease (CHD) is angina. Angina is chest pain or discomfort that occurs if an area of your heart muscle doesn't get enough oxygen-rich blood.
Angina may feel like pressure or squeezing in your chest. You also may feel it in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion. The pain tends to get worse with activity and go away with rest. Emotional stress also can trigger the pain.
Another common symptom of CHD is shortness of breath. This symptom occurs if CHD causes heart failure. When you have heart failure, your heart can't pump enough blood to meet your body’s needs. Fluid builds up in your lungs, making it hard to breathe.
The severity of these symptoms varies. They may get more severe as the buildup of plaque continues to narrow the coronary arteries.
Signs and Symptoms of Heart Problems Related to Coronary Heart Disease
Some people who have CHD have no signs or symptoms—a condition called silent CHD. The disease might not be diagnosed until a person has signs or symptoms of a heart attack, heart failure, or an arrhythmia (an irregular heartbeat).
Heart Attack
A heart attack occurs if the flow of oxygen-rich blood to a section of heart muscle is cut off. This can happen if an area of plaque in a coronary artery ruptures (breaks open).
Blood cell fragments called platelets stick to the site of the injury and may clump together to form blood clots. If a clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn’t treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
Heart With Muscle Damage and a Blocked Artery
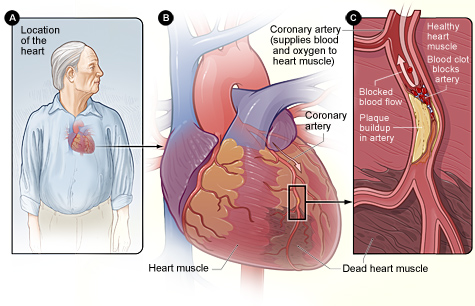
Figure A shows the location of the heart in the body. Figure B is an overview of a heart and coronary artery showing damage (dead heart muscle) caused by a heart attack. Figure C is a cross-section of the coronary artery with plaque buildup and a blood clot.
The most common heart attack symptom is chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest that often lasts for more than a few minutes or goes away and comes back.
The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain. The feeling can be mild or severe. Heart attack pain sometimes feels like indigestion or heartburn.
The symptoms of angina can be similar to the symptoms of a heart attack. Angina pain usually lasts for only a few minutes and goes away with rest.
Chest pain or discomfort that doesn’t go away or changes from its usual pattern (for example, occurs more often or while you’re resting) might be a sign of a heart attack. If you don’t know whether your chest pain is angina or a heart attack, call 9–1–1.
All chest pain should be checked by a doctor.
Other common signs and symptoms of a heart attack include:
- Upper body discomfort in one or both arms, the back, neck, jaw, or upper part of the stomach
- Shortness of breath, which may occur with or before chest discomfort
- Nausea (feeling sick to your stomach), vomiting, light-headedness or fainting, or breaking out in a cold sweat
- Sleep problems, fatigue (tiredness), or lack of energy
Heart Failure
Heart failure is a condition in which your heart can't pump enough blood to meet your body’s needs. Heart failure doesn't mean that your heart has stopped or is about to stop working.
The most common signs and symptoms of heart failure are shortness of breath or trouble breathing; fatigue; and swelling in the ankles, feet, legs, stomach, and veins in the neck.
All of these symptoms are the result of fluid buildup in your body. When symptoms start, you may feel tired and short of breath after routine physical effort, like climbing stairs.
Arrhythmia
An arrhythmia is a problem with the rate or rhythm of the heartbeat. When you have an arrhythmia, you may notice that your heart is skipping beats or beating too fast.
Some people describe arrhythmias as a fluttering feeling in the chest. These feelings are called palpitations (pal-pih-TA-shuns).
Some arrhythmias can cause your heart to suddenly stop beating. This condition is called sudden cardiac arrest (SCA). SCA usually causes death if it's not treated within minutes.
How Is Coronary Heart Disease Treated?
Treatments for coronary heart disease (CHD) include lifestyle changes, medicines, and medical procedures. Treatment goals may include:
- Relieving symptoms.
- Reducing risk factors in an effort to slow, stop, or reverse the buildup of plaque.
- Lowering the risk of blood clots forming. (Blood clots can cause a heart attack.)
- Widening or bypassing clogged arteries.
Preventing complications of CHD.
Lifestyle Changes
Making lifestyle changes often can help prevent or treat CHD. Lifestyle changes might be the only treatment that some people need.
Follow a Healthy Diet
A healthy diet is an important part of a healthy lifestyle. Following a healthy diet can prevent or reduce high blood pressure and high blood cholesterol and help you maintain a healthy weight.
Therapeutic Lifestyle Changes (TLC)
Your doctor may recommend TLC if you have high blood cholesterol. TLC is a three-part program that includes a healthy diet, physical activity, and weight management.
With the TLC diet, less than 7 percent of your daily calories should come from saturated fat. This kind of fat is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods.
No more than 25 to 35 percent of your daily calories should come from all fats, including saturated, trans, monounsaturated, and polyunsaturated fats.
You also should have less than 200 mg a day of cholesterol. The amounts of cholesterol and the types of fat in prepared foods can be found on the foods' Nutrition Facts labels.
Foods high in soluble fiber also are part of a healthy diet. They help prevent the digestive tract from absorbing cholesterol. These foods include:
- Whole-grain cereals such as oatmeal and oat bran
- Fruits such as apples, bananas, oranges, pears, and prunes
- Legumes such as kidney beans, lentils, chick peas, black-eyed peas, and lima beans
A diet rich in fruits and vegetables can increase important cholesterol-lowering compounds in your diet. These compounds, called plant stanols or sterols, work like soluble fiber.
A healthy diet also includes some types of fish, such as salmon, tuna (canned or fresh), and mackerel. These fish are a good source of omega-3 fatty acids. These acids may help protect the heart from blood clots and inflammation and reduce the risk of heart attack. Try to have about two fish meals every week.
You also should try to limit the amount of sodium (salt) that you eat. This means choosing low-salt and "no added salt" foods and seasonings at the table or while cooking. The Nutrition Facts label on food packaging shows the amount of sodium in the item.
Try to limit drinks that contain alcohol. Too much alcohol will raise your blood pressure and triglyceride level. (Triglycerides are a type of fat found in the blood.) Alcohol also adds extra calories, which will cause weight gain.
Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. One drink is a glass of wine, beer, or a small amount of hard liquor.
Dietary Approaches to Stop Hypertension (DASH)
Your doctor may recommend the DASH eating plan if you have high blood pressure. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart healthy and low in fat, cholesterol, and sodium.
DASH also focuses on fat-free or low-fat milk and dairy products, fish, poultry, and nuts. The DASH eating plan is reduced in red meats (including lean red meats), sweets, added sugars, and sugar-containing beverages. It's rich in nutrients, protein, and fiber.
The DASH eating plan is a good healthy eating plan, even for those who don’t have high blood pressure.
Be Physically Active
Routine physical activity can lower many CHD risk factors, including LDL ("bad") cholesterol, high blood pressure, and excess weight.
Physical activity also can lower your risk for diabetes and raise your HDL cholesterol level. HDL is the "good" cholesterol that helps prevent CHD.
Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. The more active you are, the more you will benefit.
Maintain a Healthy Weight
Maintaining a healthy weight can lower your risk for CHD. A general goal to aim for is a body mass index (BMI) of less than 25.
BMI measures your weight in relation to your height and gives an estimate of your total body fat.
A BMI between 25 and 29.9 is considered overweight. A BMI of 30 or more is considered obese. A BMI of less than 25 is the goal for preventing and treating CHD. Your doctor or other health care provider can help you set an appropriate BMI goal.
Quit Smoking
If you smoke, quit. Smoking can raise your risk for CHD and heart attack and worsen other CHD risk factors. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Manage Stress
Research shows that the most commonly reported "trigger" for a heart attack is an emotionally upsetting event—particularly one involving anger. Also, some of the ways people cope with stress—such as drinking, smoking, or overeating—aren't healthy.
Learning how to manage stress , relax, and cope with problems can improve your emotional and physical health. Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress.
Physical activity, medicine, and relaxation therapy also can help relieve stress. You may want to consider taking part in a stress management program.
Medicines
You may need medicines to treat CHD if lifestyle changes aren't enough. Medicines can:
- your heart’s workload and relieve CHD symptoms
- Decrease your chance of having a heart attack or dying suddenly
- Lower your cholesterol and blood pressure
- Prevent blood clots
- Prevent or delay the need for a procedure or surgery (for example, angioplasty or coronary artery bypass grafting (CABG))
Medicines used to treat CHD include anticoagulants (AN-te-ko-AG-u-lants), also called blood thinners; aspirin and other anticlotting medicines; ACE inhibitors; beta blockers; calcium channel blockers; nitroglycerin; glycoprotein IIb-IIIa; statins; and fish oil and other supplements high in omega-3 fatty acids.
Procedures and Surgery
You may need a procedure or surgery to treat CHD. Both angioplasty and CABG are used to treat blocked coronary arteries. You and your doctor can discuss which treatment is right for you.
Angioplasty
Angioplasty is a nonsurgical procedure that opens blocked or narrowed coronary arteries. This procedure also is called percutaneous (per-ku-TA-ne-us) coronary intervention, or PCI.
A thin, flexible tube with a balloon or other device on the end is threaded through a blood vessel to the narrowed or blocked coronary artery.
Once in place, the balloon is inflated to compress the plaque against the wall of the artery. This restores blood flow through the artery.
During the procedure, the doctor may put a small mesh tube called a stent in the artery. The stent helps prevent blockages in the artery in the months or years after angioplasty.
Coronary Artery Bypass Grafting
CABG is a type of surgery. In CABG, arteries or veins from other areas in your body are used to bypass (that is, go around) your narrowed coronary arteries. CABG can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
Cardiac Rehabilitation
Your doctor may prescribe cardiac rehabilitation (rehab) for angina or after CABG, angioplasty, or a heart attack. Almost everyone who has CHD can benefit from cardiac rehab.
Cardiac rehab is a medically supervised program that may help improve the health and well-being of people who have heart problems.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians or nutritionists, and psychologists or other mental health specialists.
Rehab has two parts:
- Exercise training: This part helps you learn how to exercise safely, strengthen your muscles, and improve your stamina. Your exercise plan will be based on your personal abilities, needs, and interests.
- Education, counseling, and training: This part of rehab helps you understand your heart condition and find ways to reduce your risk for future heart problems. The rehab team will help you learn how to cope with the stress of adjusting to a new lifestyle and deal with your fears about the future.
How Can Coronary Heart Disease Be Prevented or Delayed?
Taking action to control your risk factors can help prevent or delay coronary heart disease (CHD). Your risk for CHD increases with the number of risk factors you have.
One step you can take is to adopt a healthy lifestyle. Following a healthy diet is an important part of a healthy lifestyle.
A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, and beans and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
Be as physically active as you can. Physical activity can improve your fitness level and your health. Talk with your doctor about what types of activity are safe for you.
If you smoke, quit. Smoking can damage and tighten blood vessels and raise your risk for CHD. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
Know your family history of health problems related to CHD. If you or someone in your family has CHD, be sure to tell your doctor.
If lifestyle changes aren't enough, you also may need medicines to control your CHD risk factors. Take all of your medicines as prescribed.
How Is Coronary Heart Disease Diagnosed?
Your doctor will diagnose coronary heart disease (CHD) based on your medical and family histories, your risk factors for CHD, a physical exam, and the results from tests and procedures.
No single test can diagnose CHD. If your doctor thinks you have CHD, he or she may recommend one or more of the following tests.
EKG (Electrocardiogram)
An EKG is a simple, painless test that detects and records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage due to CHD and signs of a previous or current heart attack.
Stress Testing
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can't exercise, you may be given medicine to raise your heart rate.
When your heart is working hard and beating fast, it needs more blood and oxygen. Plaque-narrowed arteries can't supply enough oxygen-rich blood to meet your heart's needs.
A stress test can show possible signs and symptoms of CHD, such as:
- Abnormal changes in your heart rate or blood pressure
- Shortness of breath or chest pain
- Abnormal changes in your heart rhythm or your heart's electrical activity
If you can't exercise for as long as what is considered normal for someone your age, your heart may not be getting enough oxygen-rich blood. However, other factors also can prevent you from exercising long enough (for example, lung diseases, anemia, or poor general fitness).
As part of some stress tests, pictures are taken of your heart while you exercise and while you rest. These imaging stress tests can show how well blood is flowing in your heart and how well your heart pumps blood when it beats.
Echocardiography
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The picture shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can show areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
Chest X Ray
A chest x ray takes pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels.
A chest x ray can reveal signs of heart failure, as well as lung disorders and other causes of symptoms not related to CHD.
Blood Tests
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels might be a sign that you're at risk for CHD.
Electron-Beam Computed Tomography
Electron-beam computed tomography (EBCT) is a test that looks for specks of calcium (called calcifications) in the walls of the coronary arteries. Calcifications are an early sign of CHD.
The test can show whether you're at increased risk for a heart attack or other heart problems before other signs and symptoms occur.
EBCT isn't routinely used to diagnose CHD because its accuracy isn't yet known.
Coronary Angiography and Cardiac Catheterization
Your doctor may recommend coronary angiography (an-jee-OG-rah-fee) if other tests or factors show that you're likely to have CHD. This test uses dye and special x rays to show the insides of your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-eh-ter-ih-ZA-shun).
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through your coronary arteries. The dye lets your doctor study the flow of blood through your heart and blood vessels.
Cardiac catheterization usually is done in a hospital. You're awake during the procedure. It usually causes little or no pain, although you may feel some soreness in the blood vessel where your doctor inserts the catheter.